Chronic ulcers are wounds that don’t heal normally or go through the usual phases of healing. In simple terms, they are sores on the skin that linger for months or even years. Unlike a regular cut or scrape that closes in a few weeks, a chronic ulcer stubbornly stays open. This can happen due to underlying issues like poor circulation, diabetes, or pressure on the skin. In Kerala and around the world, proper chronic ulcer management is important because these wounds can significantly affect quality of life and lead to serious complications.
At TRIVES Hospital in Kerala, we understand how frustrating and painful chronic ulcers can be. Our goal is to help patients heal and regain normal activity through compassionate care and advanced treatments. This guide will explain what chronic ulcers are, how they are caused and diagnosed, and what you can do to manage and prevent them. We will also highlight how TRIVES Hospital’s vascular specialists and wound care experts provide comprehensive chronic ulcer management in Kerala.
What Are Chronic Ulcers?
A chronic ulcer (or chronic wound) is simply a wound that fails to heal in a normal way. Normally, a cut or ulcer goes through stages of healing—cleaning, tissue growth, and remodeling. But chronic ulcers get stuck in the early (inflammatory) stage. Doctors often say a wound that doesn’t improve after 4–6 weeks (or 3 months in some definitions) is chronic. Chronic ulcers are common on the legs and feet, but they can occur anywhere on the body.
Common examples include leg ulcers (on the lower leg), diabetic foot ulcers, pressure sores (bedsores), and arterial or ischemic ulcers. A simple way to recognize a chronic ulcer is a sore that keeps leaking fluid, maybe has dead (necrotic) tissue, and just won’t close despite care. It may hurt, itch, or develop an odor if infected. Sometimes the edges of the wound become thick or calloused. Chronic ulcers can last for months or years if not treated properly.
Common Causes of Chronic Ulcers
Chronic ulcers usually form because something is interfering with the normal healing process. Some of the most common causes are:
-
Poor blood flow (circulation problems) – When blood doesn’t flow well to an area, the skin can’t get enough oxygen and nutrients to heal. This happens with venous insufficiency (leaky leg veins) or peripheral artery disease (PAD) (narrowed arteries). For example, chronic venous insufficiency (damaged vein valves) causes blood to pool in the legs. This increases pressure in the tiny capillaries and can break the skin, leading to an ulcer. Similarly, PAD (often from diabetes or smoking) causes arteries to clog, starving the skin of blood. High blood pressure can even cause painful leg ulcers (Martorell ulcers) by damaging skin blood vessels.
-
Diabetes – High blood sugar can damage nerves (causing neuropathy) and blood vessels. People with diabetes may not feel cuts or blisters on their feet, and injuries can go unnoticed and worsen. Diabetes also slows wound healing. As one Johns Hopkins guide notes, about 25% of people with diabetes will develop a foot ulcer at some point. In Kerala, where diabetes is common, chronic diabetic foot ulcers are a frequent problem.
-
Pressure or trauma – Constant pressure on one spot (like from lying in bed or ill-fitting shoes) can cause pressure ulcers. For example, bedridden patients or wheelchair users often develop ulcers on heels, hips, or the tailbone from pressure and friction. Minor injuries or repeated trauma to an area (such as a poorly healing cut) can also turn into a chronic ulcer.
-
Infections and other conditions – Sometimes a wound becomes a chronic ulcer because it gets repeatedly infected. Skin diseases like vasculitis or autoimmune conditions can also lead to non-healing ulcers. Even radiation therapy (for cancer) can cause tissue damage that results in slow-healing wounds (radiation ulcers).
In many cases, chronic ulcers have multiple causes at once. For example, an elderly patient with varicose veins, diabetes, and limited mobility is at very high risk. The key idea is that any factor that reduces blood flow, nerves, or the body’s healing ability can turn a simple sore into a chronic one.
Types of Chronic Ulcers
There are several types of chronic ulcers, often named by their cause or location. Some main types include:
-
Venous (Stasis) Ulcers – These occur when the leg veins can’t return blood to the heart efficiently. They are often found around the inner ankles. The skin may look leathery or brownish (due to iron buildup) around the ulcer. Venous ulcers can be associated with varicose veins.
-
Arterial (Ischemic) Ulcers – Caused by poor arterial blood flow (PAD). They typically appear on the feet or toes, or pressure points like the heel. The wound edges are often well-defined and the base may look pale or punched-out. These ulcers usually hurt, especially when the leg is raised or at night.
-
Diabetic Foot Ulcers – A complication of diabetes, often on the bottom of the foot. They result from a combination of nerve damage (so you don’t feel the injury) and circulation problems. These can become infected easily.
-
Pressure Ulcers (Bedsores) – Occur from constant pressure, usually over bony areas (heels, tailbone, elbows) when lying or sitting too long in one position.
-
Neuropathic Ulcers – Caused mainly by nerve damage (diabetic neuropathy, for example). The lack of feeling leads to unnoticed injuries. Diabetic foot ulcers are a type of neuropathic ulcer.
-
Traumatic Ulcers – From burns, cuts, or other injuries that didn’t heal properly.
-
Other – Less common are radiation ulcers (from cancer treatment) or ulcers from infections or skin diseases.
Each type may look or feel a bit different, but they all share the stubborn, non-healing nature of chronic ulcers. It’s important to identify the type because treatment often targets the root cause (e.g. improving artery flow for ischemic ulcers, using compression for venous ulcers).
Symptoms and Signs
Chronic ulcers often start as a sore or wound that fails to improve over weeks. You might notice the following signs:
-
A wound or sore on the leg, foot, or other area that does not heal or keeps coming back.
-
The ulcer may have red, purple, brown or yellow tissue around it. The skin around it can look discolored or thick.
-
Fluid or discharge (clear, bloody, or yellowish) from the ulcer, especially if it’s infected.
-
Pain or discomfort – Some ulcers are painful, especially arterial ones. Venous ulcers can cause dull aches or heavy feelings in the legs.
-
Swelling and itching – Legs or feet may swell (edema) and the skin may feel tight, dry or itchy.
-
Odor – If the ulcer is infected, it may give off a foul smell.
-
Heat or redness – Inflammation can make the area warm, red, or tender to touch.
-
In severe cases, fever or redness spreading up the leg can indicate serious infection.
Often the first clue is simply “a sore on my leg won’t go away.” A helpful rule is that any leg wound not healing after two weeks should be checked by a doctor. Chronic ulcers need special wound care; ignoring them can lead to complications.
Risk Factors
Certain conditions and lifestyles make chronic ulcers more likely. Key risk factors include:
-
Age – Older adults have thinner skin, weaker circulation, and heal slower. They are much more prone to leg ulcers.
-
Diabetes – As mentioned, diabetes (especially if uncontrolled) greatly increases risk.
-
Obesity – Extra weight strains leg veins and joints, contributing to ulcers.
-
Poor circulation – Varicose veins, PAD (artery disease), and hypertension are major risk factors.
-
Smoking – Smoking damages blood vessels and impairs healing.
-
Inactivity or immobility – Long periods of sitting or lying down (post-surgery, paralysis, or sedentary job) can cause pressure ulcers and venous pooling.
-
History of ulcers – Once you have one ulcer, another often follows. Previous injury or surgery on the legs can also increase risk.
-
Foot problems – Foot deformities or poorly fitting shoes can create pressure points and sores.
-
Health conditions – Other issues like heart disease, obesity, or rheumatoid arthritis can also be contributing factors.
In Kerala, where diabetes and vascular diseases are common, many people face these risk factors. For example, studies in Kerala show a high prevalence of peripheral vascular disease in diabetic patients. This means experts like those at TRIVES must be vigilant in identifying and managing ulcers in at-risk patients.
Diagnosis and Tests
If you have a suspected chronic ulcer, a specialist (often a vascular doctor or wound care physician) will examine you carefully. Diagnosis usually involves:
-
Medical history and exam – The doctor will ask about how long the wound has been there, any injuries, pain level, and symptoms. They will look at the wound’s size, depth, and surrounding skin.
-
Vascular tests – For leg ulcers, a key test is the Ankle-Brachial Index (ABI). This uses an ultrasound probe (Doppler) to compare blood pressure in the ankle versus the arm. It checks for artery blockages or poor blood flow. TRIVES Hospital, for example, offers advanced vascular lab tests like ABI, Doppler ultrasound, and even perfusion imaging.
-
Doppler ultrasound – This non-invasive scan checks blood flow in arteries and veins. It helps find narrowed arteries or clots in veins.
-
Blood tests – Blood sugar (for diabetes), cholesterol, kidney function, and infection markers may be checked.
-
Wound culture or biopsy – If infection is suspected, a small sample of tissue or fluid from the ulcer might be sent to the lab. This can reveal bacteria or tell if a skin disease is causing the ulcer.
-
Other imaging – In some cases, angiography (dye X-ray), MR angiogram, or CT scan of blood vessels helps plan treatment, especially if surgery is considered.
-
Neuropathy assessment – Checking for nerve sensation (e.g. monofilament test in diabetic foot) can be part of the exam.
The goal of diagnosis is to understand the underlying cause (venous, arterial, diabetic, pressure, etc.) so treatment can be tailored. For example, if tests show poor artery flow, revascularization might be needed. If venous insufficiency is found, compression therapy will be key. Trained vascular teams at TRIVES use a combination of these diagnostic tools to create a clear picture of the patient’s condition.
Treatment Options
Treating a chronic ulcer usually means both local wound care and addressing underlying causes. Treatment is often multidisciplinary, combining wound care nurses, vascular surgeons, and other specialists. Key treatment steps include:
-
Wound Cleaning and Debridement – The wound must be cleaned of any bacteria, pus, or dead tissue. This can involve gentle irrigation, medical-grade solutions, or debridement (removal of dead tissue). Regular debridement helps stimulate healthy healing. TRIVES’s chronic wound program emphasizes advanced wound debridement and infection control in every case.
-
Moisture Control (Moist Healing) – Modern wound care keeps the ulcer bed moist (not dry or overly wet). Moist wound-healing techniques speed recovery and reduce scarring. Specialized dressings (hydrogels, foam, alginates, etc.) are used to maintain a balanced moisture level. This also helps control bacteria. In fact, studies show that optimal moist wound environments reduce inflammation and help new tissue grow faster.
-
Dressings and Bandages – Choosing the right dressing depends on the ulcer type and exudate (drainage) level. Some dressings release substances like silver (for infection) or hydrocolloids (for moisture). TRIVES’s team stays updated with the latest evidence-based dressings. They also ensure the wound is regularly inspected and the dressing changed on schedule.
-
Infection Control – If an infection is present (redness, warmth, foul discharge), antibiotics are used. The wound may be swabbed for culture to pick the best antibiotic. Topical antiseptics might be applied directly. Early infection control prevents an ulcer from worsening into cellulitis or sepsis.
-
Offloading and Pressure Relief – For diabetic foot ulcers or pressure sores, relieving pressure is crucial. This might mean using special footwear, casts, or cushions. For example, diabetic foot ulcers often require therapeutic shoes or total contact casts to take weight off the sore. Bedsores heal faster when the patient is frequently repositioned and high-pressure areas are padded.
-
Compression Therapy – Venous ulcers usually require compression (stockings or bandages) to improve blood flow. Compression helps push blood back up the leg and reduces swelling. It’s a cornerstone of venous ulcer care, as noted by guidelines.
-
Surgical and Interventional Treatments – If the ulcer is due to vascular problems, procedures to restore circulation may be needed. These include:
-
Angioplasty or Bypass – For arterial ulcers, angioplasty (balloon stents) or bypass surgery can re-open blocked arteries.
-
Vein Procedures – For venous ulcers, treatments like endovenous laser ablation (EVLA) or radiofrequency ablation (RFA) close off faulty veins and direct blood into healthy ones. Varicose veins or venous reflux might be surgically corrected.
-
Skin Grafts or Flaps – For large or deep ulcers, skin grafts (taking a patch of skin from another site) or muscle/fat flaps may be used to cover the wound. This is common in specialized wound centers for non-healing ulcers.
-
Minor Amputation – In severe cases where tissue is gangrenous or life is at risk, removing the affected toe or part of the foot may be necessary as a last resort.
-
-
Advanced Therapies – For difficult ulcers, newer technologies help:
-
Negative-Pressure Wound Therapy (NPWT) – Also known as vacuum-assisted closure, NPWT uses a sealed dressing with gentle suction to draw out fluids and promote tissue growth. TRIVES Hospital’s wound care program offers NPWT as an option for eligible ulcers.
-
Hyperbaric Oxygen Therapy (HBOT) – This involves breathing 100% oxygen in a pressurized chamber, which can increase oxygen delivery to tissues. Some patients with diabetic or radiation ulcers benefit from HBOT. TRIVES lists hyperbaric therapy among its services for complex ulcers.
-
Bioengineered Skin Substitutes – These are lab-grown skin tissues or matrices applied to chronic wounds to stimulate healing. TRIVES is equipped to use advanced skin substitutes in hard-to-heal cases.
-
Growth Factors and Stem Cells – Experimental treatments like platelet-rich plasma or cellular therapies are on the horizon and used in specialized centers.
-
-
Medications – Besides antibiotics, certain medications can help heal ulcers. For instance, vasodilators (to widen blood vessels), or drugs to improve circulation. Pain management is also important to keep the patient comfortable.
-
Nutrition and Support – Good nutrition (especially enough protein, vitamins, and minerals) is vital for healing. A dietitian may ensure the patient eats well. Stopping smoking is critical, as tobacco severely impairs wound healing.
TRIVES Hospital’s Expertise in Chronic Ulcer Care
At TRIVES Hospital, we are proud to be Kerala’s first and only exclusive vascular hospital. This means our entire focus is on blood vessel health and related conditions, including chronic ulcers. Here’s what sets us apart in chronic ulcer management:
-
Specialized Vascular Team – Our board-certified vascular surgeons and specialist nurses are experts in treating circulation problems and ulcers. They work together in a multidisciplinary team (with podiatrists, dermatologists, infectious disease specialists, etc.) to create personalized treatment plans.
-
State-of-the-Art Diagnostics – We have advanced Doppler ultrasound machines, a dedicated vascular laboratory, and imaging systems for ABI and perfusion studies. Accurate diagnosis of blood flow issues is crucial to healing ulcers.
-
Comprehensive Wound Center – TRIVES combines vascular care with diabetic foot care in one center. Our Vascular & Diabetic Foot Centre offers specialized podiatry services (foot screenings, orthotic fittings, nail care) and a chronic wound program.
-
Advanced Treatment Options – As noted, we offer hyperbaric oxygen therapy, negative-pressure wound therapy, and bioengineered skin treatments. These advanced modalities are not available everywhere, so Kerala patients benefit from having them at TRIVES.
-
Clinical Protocols – Our chronic wound management includes strict infection control protocols. We use specialized compression therapy systems for venous ulcers and monitor tissue oxygen levels (TcPO₂) to guide healing.
-
Multidisciplinary Approach – Beyond wound care, we address root causes. Our varicose vein clinic performs modern procedures like radiofrequency ablation (RFA) and VenaSeal for venous insufficiency. Our angioplasty and vascular surgery teams treat arterial disease aggressively to restore limb circulation.
-
Cutting-Edge Facilities – The hospital has high-tech operating theaters and ICU units for complex cases. We operate 24/7 emergency care, advanced imaging, and in-house labs to support urgent wound cases or surgeries.
-
Experienced Specialists – For example, Dr. Vineeth Kumar PM, a consultant vascular surgeon trained at top institutions, leads our team. We stay up-to-date with the latest evidence-based guidelines and research.
-
Patient-Centered Care – We believe in compassionate care. From the first consultation to follow-ups, we educate patients and families about wound care and prevention. Our nursing staff is trained in chronic wound management and often provides at-home care instructions.
Figure: Expert care at TRIVES Hospital. Our vascular surgeons (shown here in surgery) and wound care team use advanced techniques and compassionate care to heal chronic ulcers.
By integrating all these strengths, TRIVES Hospital offers one of the most comprehensive chronic ulcer management programs in Kerala. Whether the ulcer is due to diabetes, varicose veins, or arterial disease, TRIVES’s multidisciplinary team has the expertise to help. We follow every patient closely, using evidence-based protocols and modern technologies to give the best chance of healing.
Lifestyle Modifications for Healing and Prevention
In addition to medical treatments, certain lifestyle steps can greatly help chronic ulcer patients heal and prevent new ulcers:
-
Daily Skin and Foot Care – Check your skin (especially feet and legs) every day for cuts, blisters, or redness. People with diabetes should inspect their feet meticulously and use a mirror or ask for help if needed. Early detection of a small problem (a callus or minor cut) allows prompt care before it becomes an ulcer.
-
Proper Footwear and Clothing – Always wear well-fitting shoes with adequate support and toe room. Avoid tight socks or shoes that cause friction. Use breathable, soft socks. At home, use slippers with padding. For leg ulcers, avoid tight stockings or clothing that might cut off circulation.
-
Maintain Good Blood Sugar Levels – For diabetic patients, keeping blood sugar in the target range is crucial. High blood sugar impairs healing. Work with your doctor to monitor and manage diabetes; medications or insulin may need adjustment.
-
Healthy Diet and Weight – Eat a balanced diet rich in protein, vitamins (especially A and C), and minerals like zinc, which help wound healing. Maintain a healthy weight; extra pounds strain leg veins and joints. In obese patients, weight loss can improve circulation and make wound care easier.
-
Stay Active and Elevate Legs – Do gentle exercises (like walking) as advised by your doctor to improve circulation. Leg elevation is recommended for venous ulcers: when sitting or lying down, raise your legs above heart level for periods each day to reduce swelling.
-
Compression Stockings – If you have venous insufficiency or a healed venous ulcer, wearing prescription compression stockings can prevent recurrence. This should be discussed with your doctor.
-
Quit Smoking – Tobacco slows healing by narrowing blood vessels. Quitting smoking or any tobacco is one of the best things you can do for ulcer healing.
-
Hydration and Skin Care – Keep the skin around at-risk areas clean and well-moisturized with gentle lotions. Dry, cracked skin is more prone to ulcers. Use non-irritating soaps and lotions, especially in the winter or dry climate.
-
Manage Health Conditions – Keep conditions like high blood pressure and cholesterol under control with diet, exercise, and medications. These factors affect blood flow and healing.
-
Attend Follow-Up Appointments – Regular check-ups with your vascular or wound care team ensure any small issue is caught early. Don’t skip appointments, even if the wound is improving.
In short, preventing ulcers involves caring for your legs and feet daily, staying healthy, and avoiding trauma. As the Cleveland Clinic notes, leg ulcers often recur, but measures like leg elevation, exercise, and compression can reduce the risk of new ulcers. Similarly, NYU Langone advises diabetic patients to take care of any foot injury promptly and manage blood sugar to speed healing.
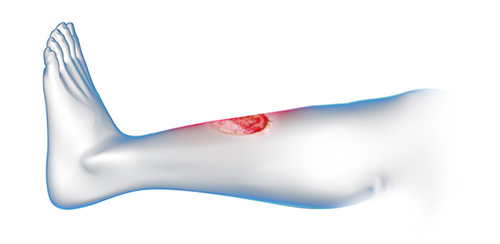
Figure: Early care prevents chronic wounds. Proper first aid and bandaging of an injury (as shown) can stop a small wound from turning into a chronic ulcer.
Patient Care and Support
Living with a chronic ulcer can be challenging, so patient care and education are key parts of treatment. At TRIVES Hospital, we emphasize the “whole patient” approach. This means:
-
Education – We teach you and caregivers about wound hygiene, dressing changes, and recognizing signs of infection. Studies show patient and caregiver education is an essential component of wound care.
-
Home Care Instructions – Our nurses will demonstrate how to keep your wound clean at home, how to apply dressings (if needed), and how to wear compression properly. We provide written instructions and educational materials.
-
Pain Management – Chronic ulcers can be painful. We address pain with medications or therapies like elevation and gentle movement. Effective pain control helps you stay active and follow care plans.
-
Nutrition and Lifestyle Counseling – Dietitians counsel patients on a healthy diet that supports healing. We might recommend supplements if nutrition is poor.
-
Psychosocial Support – Long-term wounds can affect mood. We encourage family involvement and, if needed, referrals to counseling or support groups.
-
Physical Therapy – If mobility is affected (e.g., from a foot ulcer or amputation risk), we work with physiotherapists to keep you moving safely. Exercise helps circulation and overall health.
-
Wound Clinics and Telemedicine – We offer dedicated wound care clinics where we can review the ulcer regularly. For those unable to travel, TRIVES provides telemedicine support, where patients send photos and video consultations to stay on track.
-
Preventing Complications – We stay vigilant for complications. People with ulcers are at risk for cellulitis, bone infections (osteomyelitis), and even sepsis. Our team watches for fever, increased pain, or spreading redness. Early intervention can prevent serious outcomes like amputation. In fact, an open ulcer has a high risk of infection, which can spread to bone and may require surgery if not treated.
-
Follow-Up – Once an ulcer heals, we still monitor you. Ulcers can recur, so preventive care and check-ups continue even after closure.
By providing education, emotional support, and a structured care plan, we help patients manage life with a chronic ulcer. The goal is not only to heal the wound but also to keep it from coming back, which means addressing lifestyle and health factors comprehensively.
Prevention Tips
Preventing chronic ulcers or their recurrence is often easier than healing them. Key tips include:
-
Daily Skin Checks – Look for any new wounds, especially on feet and legs. Even a small blister can become a problem if ignored.
-
Good Hygiene – Keep skin clean and dry. Use mild soap and avoid harsh chemicals.
-
Protect Your Skin – Use protective padding or bandages on areas prone to pressure or friction.
-
Wear Proper Footwear – As noted, comfortable shoes and socks are crucial.
-
Use Compression if Advised – If you had a venous ulcer, wearing doctor-prescribed compression stockings can prevent recurrence.
-
Elevate Your Legs – Lie down and prop your legs up above heart level several times a day. This simple habit reduces leg swelling.
-
Stay Active – Even gentle walking boosts circulation. Bedrest should be avoided if possible.
-
Maintain Health – Control diabetes, hypertension, and cholesterol through medication, diet, and exercise.
-
Quit Smoking – Seek help to stop smoking, as it dramatically improves blood flow and healing prospects.
-
Hydration and Diet – Drink enough water and eat a diet rich in vegetables, fruits, and protein to support skin health.
-
Avoid Prolonged Pressure – If bedridden, change positions often. Use cushions to relieve pressure on hips, heels, and other vulnerable areas.
-
Be Cautious with Foot Care – Avoid walking barefoot, even at home. Never trim corns or calluses yourself.
Following these steps can significantly lower the chances of developing an ulcer or getting another one. Remember that chronic ulcers often come back – the Cleveland Clinic notes that taking preventive steps (like elevation, lifestyle management, and weight control) lowers the risk of getting a leg ulcer again.
Conclusion and How TRIVES Can Help
Chronic ulcers may be stubborn, but with the right care they can heal and be prevented in the future. Key points to remember:
-
Chronic ulcers are wounds that won’t heal normally. They often result from circulation problems, diabetes, or pressure.
-
Symptoms include a persistent sore with possible discharge, color changes, and pain.
-
Risk factors include diabetes, vascular disease, immobility, obesity, and smoking.
-
Diagnosis often requires vascular testing (ABI, Doppler) and sometimes biopsy.
-
Treatment is multi-faceted: cleaning, dressings, compression, offloading, medication, and sometimes surgery (vein fixes, angioplasty, grafts).
-
Advanced therapies like hyperbaric oxygen and NPWT can boost healing for hard ulcers.
-
Prevention revolves around good foot care, proper footwear, leg elevation, exercise, and controlling health conditions.
-
Education and patient support are vital for long-term success.
If you or someone you care about is dealing with a chronic ulcer, help is available right here in Kerala. TRIVES Hospital offers expert chronic ulcer management through our Vascular & Diabetic Foot Centre. We bring together the latest technology, skilled surgeons, and compassionate care all under one roof. Our team will perform a thorough evaluation and tailor a treatment plan just for you.
Don’t let a stubborn wound go untreated—early intervention leads to the best outcomes. Call TRIVES Hospital today at +91 9495292866, +91 9495292101 to book a consultation. You can also visit our website www.trives.in to schedule an appointment online. Our friendly staff is ready to answer your questions and guide you on the path to healing.
Trust TRIVES Hospital for chronic ulcer management in Kerala. We are committed to healing, one wound at a time, so you can get back to enjoying life without pain or worry.
Frequently Asked Questions
1. What is a chronic ulcer?
A chronic ulcer is a wound that hasn’t healed within three months and often gets stuck in the inflammatory stage. TRIVES Hospital specializes in evaluating and treating these non-healing wounds to kick-start the healing process.
2. What are the main causes of chronic ulcers?
Chronic ulcers most often result from poor blood flow (venous insufficiency or peripheral artery disease), diabetes-related nerve damage, or constant pressure on the skin. At TRIVES Hospital, our team addresses each underlying cause with targeted vascular and wound-care treatments.
3. How are chronic ulcers diagnosed?
Diagnosis includes a physical exam of the wound, Ankle-Brachial Index (ABI) testing, Doppler ultrasound, blood tests, and sometimes wound cultures. TRIVES Hospital’s state-of-the-art vascular lab performs these assessments to create a personalized care plan.
4. What non-surgical treatments are available?
Non-surgical options include wound cleaning and debridement, moist-healing dressings, compression therapy for venous ulcers, and offloading devices for diabetic foot ulcers. TRIVES Hospital’s wound-care nurses are trained in the latest protocols for optimal healing.
5. When is surgery needed for chronic ulcers?
Surgery is considered if conservative measures fail or if blood flow must be restored. Procedures include angioplasty, bypass surgery, endovenous ablation, skin grafts, or minor amputation. TRIVES Hospital’s vascular surgeons perform these advanced interventions in dedicated operating rooms.
6. What advanced therapies can help with healing?
Advanced options include negative-pressure wound therapy (NPWT), hyperbaric oxygen therapy (HBOT), bioengineered skin substitutes, and growth-factor treatments. TRIVES Hospital offers NPWT and HBOT as part of its comprehensive chronic ulcer program.
7. How important is infection control in ulcer management?
Infection can delay healing and cause serious complications. Wound cultures guide targeted antibiotics and antiseptics. TRIVES Hospital follows strict infection-control protocols to keep ulcers free of harmful pathogens.
8. What lifestyle changes support ulcer healing and prevention?
Key steps include daily skin and foot inspections, proper footwear, leg elevation, smoking cessation, good blood sugar control, and a balanced diet. TRIVES Hospital’s team provides personalized education to help patients adopt these healthy habits.
9. How long does it take for a chronic ulcer to heal?
Healing time varies by ulcer type and cause. Venous leg ulcers often heal within 6 months with proper compression, while diabetic foot ulcers may take weeks to months. TRIVES Hospital monitors progress closely and adjusts treatment plans to optimize healing.
10. How can I make an appointment at TRIVES Hospital for chronic ulcer care?
To book a consultation with our vascular and wound-care specialists, call +91 9495292866, +91 9495292101 , or visit www.trives.in and complete the online enquiry form.


